20200907 Anorexia nervosa
Monday, 07 September
#Today I still wanna write about another eating disorder. It was Anorexia.
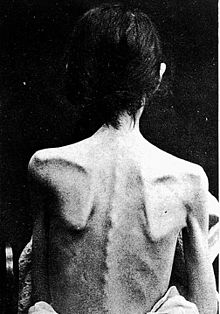
https://images.app.goo.gl/hcHu1hXkThWqz9az6
Anorexia nervosa, often referred to simply as anorexia, is an eating disorder, characterized by low weight, food restriction, fear of gaining weight, and a strong desire to be thin. Many people with anorexia see themselves as overweight even though they are, in fact, underweight. They often deny that they have a problem with low weight. They weigh themselves frequently, eat small amounts, and only eat certain foods. Some exercise excessively, force themselves to vomit, or use laxatives to produce weight loss. Complications may include osteoporosis, infertility, and heart damage, among others. Women will often stop having menstrual periods. In extreme cases, people with anorexia who continually refuse significant dietary intake and weight restoration interventions may be fed by force under restraint via nasogastric tube within specialist psychiatric hospitals.
The cause is currently unknown. There appear to be some genetic components with identical twins more often affected than fraternal twins. Cultural factors also appear to play a role, with societies that value thinness having higher rates of disease. Additionally, it occurs more commonly among those involved in activities that value thinness, such as high-level athletics, modelling, and dancing. Anorexia often begins following a major life-change or stress-inducing event. The diagnosis requires a significantly low weight. The severity of disease is based on Body Mass Index (BMI) in adults with mild disease having a BMI of greater than 17, moderate a BMI of 16 to 17, severe a BMI of 15 to 16, and extreme a BMI less than 15. In children a BMI for age percentile of less than the 5th percentile is often used.
Treatment of anorexia involves restoring a healthy weight, treating the underlying psychological problems, and addressing behaviors that promote the problem. While medications do not help with weight gain, they may be used to help with associated anxiety or depression. A number of types of therapy may be useful, such as cognitive behavioral therapy or an approach where parents assume responsibility for feeding their child known as Maudsley family therapy. times people require admission to a hospital to restore weight. Evidence for benefit from nasogastric tube feeding, however is unclear; such an intervention may be highly distressing for both anorexia patients and healthcare staff when administered against the patient's will under restraint. Some people with anorexia will just have a single episode and recover while others may have many episodes over years. Many complications improve or resolve with regaining of weight.
Globally, anorexia is estimated to affect 2.9 million people as of 2015. It is estimated to occur in 0.9% to 4.3% of women and 0.2% to 0.3% of men in Western countries at some point in their life. About 0.4% of young women are affected in a given year and it is estimated to occur ten times more commonly among women than men. Rates in most of the developing world are unclear. Often it begins during the teen years or young adulthood. While anorexia became more commonly diagnosed during the 20th century it is unclear if this was due to an increase in its frequency or simply better diagnosis. In 2013 it directly resulted in about 600 deaths globally, up from 400 deaths in 1990. Eating disorders also increase a person's risk of death from a wide range of other causes, including suicide. About 5% of people with anorexia die from complications over a ten-year period, a nearly six times increased risk. The term "anorexia nervosa" was first used in 1873 by William Gull to describe this condition.
Anorexia nervosa is an eating disorder characterized by attempts to lose weight, to the point of starvation. A person with anorexia nervosa may exhibit a number of signs and symptoms, the type and severity of which may vary and may be present but not readily apparent.
Anorexia nervosa, and the associated malnutrition that results from self-imposed starvation, can cause complications in every major organ system in the body. Hypokalemia, a drop in the level of potassium in the blood, is a sign of anorexia nervosa. A significant drop in potassium can cause abnormal heart rhythms, constipation, fatigue, muscle damage and paralysis.
Symptoms may include:
- A low body mass index for one's age and height.
- Amenorrhea, a symptom that occurs after prolonged weight loss; causing menstruation to stop, hair to become brittle, and skin to become yellow and unhealthy.
- Fear of even the slightest weight gain; taking all precautionary measures to avoid weight gain or becoming "overweight".
- Rapid, continuous weight loss.
- Lanugo: soft, fine hair growing over the face and body.
- An obsession with counting calories and monitoring fat contents of food.
- Preoccupation with food, recipes, or cooking; may cook elaborate dinners for others, but not eat the food themselves or consume a very small portion.
- Food restrictions despite being underweight or at a healthy weight.
- Food rituals, such as cutting food into tiny pieces, refusing to eat around others and hiding or discarding of food.
- Purging: May use laxatives, diet pills, ipecac syrup, or water pills to flush food out of their system after eating or may engage in self-induced vomiting though this is a more common symptom of Bulimia.
- Excessive exercise including micro-exercising, for example making small persistent movements of fingers or toes.
- Perception of self as overweight, in contradiction to an underweight reality.
- Intolerance to cold and frequent complaints of being cold; body temperature may lower (hypothermia) in an effort to conserve energy due to malnutrition.
- Hypotension or orthostatic hypotension.
- Bradycardia or tachycardia.
- Depression, anxiety disorders and insomnia.
- Solitude: may avoid friends and family and become more withdrawn and secretive.
- Abdominal distention.
- Halitosis (from vomiting or starvation-induced ketosis).
- Dry hair and skin, as well as hair thinning.
- Chronic fatigue.
- Rapid mood swings.
- Having feet discoloration causing an orange appearance.
- Having severe muscle tension, aches and pains.
- Evidence/habits of self harming or self-loathing.
- Admiration of thinner people.
- Infertility.
Interoception involves the conscious and unconscious sense of the internal state of the body, and it has an important role in homeostasis and regulation of emotions. Aside from noticeable physiological dysfunction, interoceptive deficits also prompt individuals with anorexia to concentrate on distorted perceptions of multiple elements of their body image. This exists in both people with anorexia and in healthy individuals due to impairment in interoceptive sensitivity and interoceptive awareness.
Aside from weight gain and outer appearance, people with anorexia also report abnormal bodily functions such as indistinct feelings of fullness. This provides an example of miscommunication between internal signals of the body and the brain. Due to impaired interoceptive sensitivity, powerful cues of fullness may be detected prematurely in highly sensitive individuals, which can result in decreased calorie consumption and generate anxiety surrounding food intake in anorexia patients. People with anorexia also report difficulty identifying and describing their emotional feelings and the inability to distinguish emotions from bodily sensations in general, called alexithymia.
Interoceptive awareness and emotion are deeply intertwined, and could mutually impact each other in abnormalities. Anorexia patients also exhibit emotional regulation difficulties that ignite emotionally-cued eating behaviors, such as restricting food or excessive exercising. Impaired interoceptive sensitivity and interoceptive awareness can lead anorexia patients to adapt distorted interpretations of weight gain that are cued by physical sensations related to digestion (e.g., fullness). Combined, these interoceptive and emotional elements could together trigger maladaptive and negatively reinforced behavioral responses that assist in the maintenance of anorexia. In addition to metacognition, people with anorexia also have difficulty with social cognition including interpreting others’ emotions, and demonstrating empathy. Abnormal interoceptive awareness and interoceptive sensitivity shown through all of these examples have been observed so frequently in anorexia that they have become key characteristics of the illness.
Other psychological issues may factor into anorexia nervosa; some fulfill the criteria for a separate Axis I diagnosis or a personality disorder which is coded Axis II and thus are considered comorbid to the diagnosed eating disorder. Some people have a previous disorder which may increase their vulnerability to developing an eating disorder and some develop them afterwards. The presence of Axis I or Axis II psychiatric comorbidity has been shown to affect the severity and type of anorexia nervosa symptoms in both adolescents and adults.
Obsessive-Compulsive Disorder (OCD) and Obsessive-Compulsive Personality Disorders (OCPD) are highly comorbid with AN, particularly the restrictive subtype. OCPD is linked with more severe symptomatology and worse prognosis. The causality between personality disorders and eating disorders has yet to be fully established. Other comorbid conditions include depression, alcoholism, borderline and other personality disorders, anxiety disorders, attention deficit hyperactivity disorders and Body Dysmorphic Disorder (BDD). Depression and anxiety are the most common comorbidities, and depression is associated with a worse outcome.
Autism spectrum disorders occur more commonly among people with eating disorders than in the general population. Zucker et al. (2007) proposed that conditions on the autism spectrum make up the cognitive endophenotype underlying anorexia nervosa and appealed for increased interdisciplinary collaboration.
There is evidence for biological, psychological, developmental, and sociocultural risk factors, but the exact cause of eating disorders is unknown.
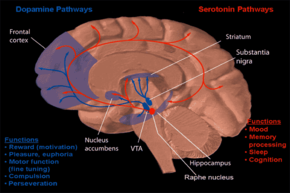
Anorexia nervosa is highly heritable. Twin studies have shown a heritability rate of between 28 and 58%. First-degree relatives of those with anorexia have roughly 12 times the risk of developing anorexia. Association studies have been performed, studying 128 different polymorphism related to 43 genes including genes involved in regulation of eating behavior, motivation and reward mechanics, personality traits and emotion. Consistent associations have been identified for polymorphisms associated with agouti-related peptide, brain derived neurotrophic factor, catechol-o-methyl transferase, SK3 and opioid receptor delta-1. Epigenetic modifications, such as DNA methylation, may contribute to the development or maintenance of anorexia nervosa, though clinical research in this area is in its infancy.
A 2019 study found a genetic relationship with mental disorders, such as schizophrenia, obsessive–compulsive disorder, anxiety disorder and depression; and metabolic functioning with a negative correlation with fat mass, type 2 diabetes and leptin.
Obstetric complications: prenatal and perinatal complications may factor into the development of anorexia nervosa, such as preterm birth, mat anemia, diabetes mellitus, preeclampsia, placenta infarction, and neonatal heart abnormalities. Neonatal complications may also have an influence on harm avoidance, one of the personality traits associated with the development of AN.
Neuroendocrine dysregulation: altered signalling of peptides that facilitate communication between the gut, brain and adipose tissue, such as ghrelin, leptin, neuropeptide Y and orexin, may contribute to the pathogenesis of anorexia nervosa by disrupting regulation of hunger and satiety.
Gastrointestinal disease: people with gastrointestinal disorders may be more at risk of developing disorders of eating practices than the general population, principally restrictive eating disturbances. An association of anorexia nervosa with celiac disease has been found. The role that gastrointestinal symptoms play in the development of eating disorders seems rather complex. Some authors report that unresolved symptoms prior to gastrointestinal disease diagnosis may create a food aversion in these persons, causing alterations to their eating patterns. Other authors report that greater symptoms throughout their diagnosis led to greater risk. It has been documented that some people with celiac disease, irritable bowel syndrome or inflammatory bowel disease who are not conscious about the importance of strictly following their diet, choose to consume their trigger foods to promote weight loss. On the other hand, individuals with good dietary management may develop anxiety, food aversion and eating disorders because of concerns around cross contamination of their foods. Some authors suggest that medical professionals should evaluate the presence of an unrecognized celiac disease in all people with eating disorder, especially if they present any gastrointestinal symptom (such as decreased appetite, abdominal pain, bloating, distension, vomiting, diarrhea or constipation), weight loss, or growth failure; and also routinely ask celiac patients about weight or body shape concerns, dieting or vomiting for weight control, to evaluate the possible presence of eating disorders, especially in women.
Studies have hypothesized the continuance of disordered eating patterns may be epiphenomena of starvation. The results of the Minnesota Starvation Experiment showed normal controls exhibit many of the behavioral patterns of AN when subjected to starvation. This may be due to the numerous changes in the neuroendocrine system, which results in a self-perpetuating cycle.
Anorexia nervosa is more likely to occur in a person's pubertal years. Some explanatory hypotheses for the rising prevalence of eating disorders in adolescence are "increase of adipose tissue in girls, hormonal changes of puberty, societal expectations of increased independence and autonomy that are particularly difficult for anorexic adolescents to meet; [and] increased influence of the peer group and its values."
Early theories of the cause of anorexia linked it to childhood sexual abuse or dysfunctional families; evidence is conflicting, and well-designed research is needed. The fear of food is known as sitiophobia, cibophobia, and is part of the differential diagnosis. Other psychological causes of anorexia include low self-esteem, feeling like there is lack of control, depression, anxiety, and loneliness.
Anorexia nervosa has been increasingly diagnosed since 1950; the increase has been linked to vulnerability and internalization of body ideals. People in professions where there is a particular social pressure to be thin (such as models and dancers) were more likely to develop anorexia, and those with anorexia have much higher contact with cultural sources that promote weight loss. This trend can also be observed for people who partake in certain sports, such as jockeys and wrestlers. There is a higher incidence and prevalence of anorexia nervosa in sports with an emphasis on aesthetics, where low body fat is advantageous, and sports in which one has to make weight for competition. Family group dynamics can play a role in the cause of anorexia. When there is a constant pressure from people to be thin, teasing and bullying can cause low self-esteem and other psychological symptoms.
Persistent exposure to media that presents body ideals may constitute a risk factor for body dissatisfaction and anorexia nervosa. The cultural ideal for body shape for men versus women continues to favor slender women and athletic, V-shaped muscular men. A 2002 review found that, of the magazines most popular among people aged 18 to 24 years, those read by men, unlike those read by women, were more likely to feature ads and articles on shape than on diet. Body dissatisfaction and internalization of body ideals are risk factors for anorexia nervosa that threaten the health of both male and female populations.
Websites that stress the importance of attainment of body ideals extol and promote anorexia nervosa through the use of religious metaphors, lifestyle descriptions, "thinspiration" or "fitspiration" (inspirational photo galleries and quotes that aim to serve as motivators for attainment of body ideals). Pro-anorexia websites reinforce internalization of body ideals and the importance of their attainment.
The media portray a false view of what people truly look like. In magazines and movies and even on billboards most of the actors/models are digitally altered in multiple ways. People then strive to look like these "perfect" role models when in reality they are not near perfection themselves.
A diagnostic assessment includes the person's current circumstances, biographical history, current symptoms, and family history. The assessment also includes a mental state examination, which is an assessment of the person's current mood and thought content, focusing on views on weight and patterns of eating.
Anorexia nervosa is classified under the Feeding and Eating Disorders in the latest revision of the Diagnostic and Statistical Manual of Mental Disorder (DSM 5). There is no specific BMI cutoff that defines low weight required for the diagnosis of anorexia nervosa.
The diagnostic criteria for anorexia nervosa (all of which needing to be meet for diagnosis) include:
- Restriction of energy intake relative to requirements leading to a low body weight.
- Intense fear of gaining weight or persistent behaviors that interfere with gaining weight.
- Disturbance in the way a person's weight or body shape is experienced or a lack of recognition about the risks of the low body weight.
Relative to the previous version of the DSM (DSM-IV-TR), the 2013 revision (DSM5) reflects changes in the criteria for anorexia nervosa, most notably that of the amenorrhea criterion being removed. Amenorrhea was removed for several reasons: it does not apply to males, it is not applicable for females before or after the age of menstruation or taking birth control pills, and some women who meet the other criteria for AN still report some menstrual activity.
There are two subtypes of AN:
- Binge-eating/purging type: the individual utilizes binge eating or displays purging behavior as a means for losing weight. It is different from bulimia nervosa in terms of the individual's weight. An individual with binge-eating/purging type anorexia can maintain a healthy or normal weight, but is usually significantly underweight. People with bulimia nervosa on the other hand can sometimes be overweight.
- Restricting type: the individual uses restricting food intake, fasting, diet pills, or exercise as a means for losing weight; they may exercise excessively to keep off weight or prevent weight gain, and some individuals eat only enough to stay alive. In the restrictive type, there are no recurrent episodes of binge-eating or purging present.
Body Mass Index (BMI) is used by the DSM-5 as an indicator of the level of severity of anorexia nervosa. The DSM-5 states these as follows:
- Mild: BMI of greater than 17
- Moderate: BMI of 16–16.99
- Severe: BMI of 15–15.99
- Extreme: BMI of less than 15
Medical tests to check for signs of physical deterioration in anorexia nervosa may be performed by a general physician or psychiatrist, including:
- Complete Blood Count (CBC): a test of the white blood cells, red blood cells and platelets used to assess the presence of various disorders such as leukocytosis, leukopenia, trhrobocytosis and anemia which may result from malnutrition.
- Urinalysis: a variety of tests performed on the urine used in the diagnosis of medical disorders, to test for substance abuse, and as an indicator of overall health.
- Chem-20: Chem-20 also known as SMA-20 a group of twenty separate chemical tests performed on bloo seru. Tests include cholesterol, protein and electrolytes such as potassium, chlorine and sodium and tests specific to liver and kidney function.
- Glucose tolerance test: Oral glucose tolerance test (OGTT) used to assess the body's ability to metabolize glucose. Can be useful in detecting various disorders such as diabetes, an insulinoma, Cushing's Syndrome, hypoglycemia and polycystic ovary syndrome.
- Serum cholinesterase test: a test of liver enzymes (acetylcholinesterase and pseudocholinesterase) useful as a test of liver function and to assess the effects of malnutrition.
- Liver Function Test: A series of tests used to assess liver function some of the tests are also used in the assessment of malnutrition, protein deficiency, kidney function, bleeding disorders, and Crohn's Disease.
- Luteinizing Hormone (LH) response to Gonadotropin-Releasing Hormone (GnRH): Tests the pituitary glands' response to GnRh, a hormone produced in the hypothalamus. Hypogonadism is often seen in anorexia nervosa cases.
- Creatine Kinase (CK) test: measures the circulating blood levels of creatine kinase an enzyme found in the heart (CK-MB), brain (CK-BB) and skeletal muscle (CK-MM).
- Blood Urea Nitrogen (BUN) test: urea nitrogen is the byproduct of protein metabolism first formed in the liver then removed from the body by the kidneys. The BUN test is primarily used to test kidney function. A low BUN level may indicate the effects of malnutrition.
- BUN-to-creatinine ratio: A BUN to creatinine ratio is used to predict various conditions. A high BUN/creatinine ratio can occur in severe hydration, acute kidney failure, congestive heart failure, and intestinal bleeding. A low BUN/creatinine ratio can indicate a low protein diet, celiac disease, rhabdomyolysis, or cirrhosis of the liver.
- Electrocardiogram (EKG or ECG): measures electrical activity of the heart. It can be used to detect various disorders such as hyperkalemia.
- Electroencephalogram (EEG): measures the electrical activity of the brain. It can be used to detect abnormalities such as those associated with pituitary tumors.
- Thyroid screen: test used to assess thyroid functioning by checking levels of thyroid-stimulating hormone (TSH), thyroxine (T4), and triiodothyronine (T3).
A variety of medical and psychological conditions have been misdiagnosed as anorexia nervosa; in some cases the correct diagnosis was not made for more than ten years.
The distinction between the diagnosis of anorexia nervosa, bulimia nervosa and eating disorder not otherwise specified (EDNOS) is often difficult to make as there is considerable overlap between people diagnosed with these conditions. Seemingly minor changes in people's overall behavior or attitude can change a diagnosis from anorexia: binge-eating type to bulimia nervosa. A main factor differentiating binge-purge anorexia from bulimia is the gap in physical weight. Someone with bulimia nervosa is ordinarily at a healthy weight, or slightly overweight. Someone with binge-purge anorexia is commonly underweight. People with the binge-purging subtype of AN may be significantly underweight and typically do not binge-eat large amounts of food, yet they purge the small amount of food they eat. In contrast, those with bulimia nervosa tend to be at normal weight or overweight and binge large amounts of food. It is not unusual for a person with an eating disorder to "move through" various diagnoses as their behavior and beliefs change over time.
There is no conclusive evidence that any particular treatment for anorexia nervosa works better than others; however, there is enough evidence to suggest that early intervention and treatment are more effective. Treatment for anorexia nervosa tries to address three main areas.
- Restoring the person to a healthy weight;
- Treating the psychological disorders related to the illness;
- Reducing or eliminating behaviours or thoughts that originally led to the disordered eating.
Although restoring the person's weight is the primary task at hand, optimal treatment also includes and monitors behavioral change in the individual as well. There is some evidence that hospitalisation might adversely affect long term outcome.
Psychotherapy for individuals with AN is challenging as they may value being thin and may seek to maintain control and resist change. Some studies demonstrate that family based therapy in adolescents with AN is superior to individual therapy. Due to the nature of the condition, treatment of people with AN can be difficult because they are afraid of gaining weight. Initially developing a desire to change is important.
Diet is the most essential factor to work on in people with anorexia nervosa, and must be tailored to each person's needs. Food variety is important when establishing meal plans as well as foods that are higher in energy density. People must consume adequate calories, starting slowly, and increasing at a measured pace. Evidence of a role for zinc supplementation during refeeding is unclear.
Family-based treatment (FBT) has been shown to be more successful than individual therapy for adolescents with AN. Various forms of family-based treatment have been proven to work in the treatment of adolescent AN including Conjoint Family Therapy (CFT), in which the parents and child are seen together by the same therapist, and separated family therapy (SFT) in which the parents and child attend therapy separately with different therapists. Proponents of family therapy for adolescents with AN assert that it is important to include parents in the adolescent's treatment.
A four- to five-year follow up study of the Maudsley family therapy, an evidence-based manualized model, showed full recovery at rates up to 90%. Although this model is recommended by the NIMH, critics claim that it has the potential to create power struggles in an intimate relationship and may disrupt equal partnerships.
There is tentative evidence that family therapy is as effective as treatment as usual and it is unclear if family therapy is more effective than educational interventions.
Cognitive Behavioral Therapy (CBT) is useful in adolescents and adults with anorexia nervosa; acceptance and commitment therapy is a type of CBT, which has shown promise in the treatment of AN. Cognitive Remediation Therapy (CRT) is used in treating anorexia nervosa.
Pharmaceuticals have limited benefit for anorexia itself. There is a lack of good information from which to make recommendations concerning the effectiveness of antidepressants in treating anorexia.
AN has a high mortality and patients admitted in a severely ill state to medical units are at particularly high risk. Diagnosis can be challenging, risk assessment may not be performed accurately, consent and the need for compulsion may not be assessed appropriately, refeeding syndrome may be missed or poorly treated and the behavioural and family problems in AN may be missed or poorly managed. The MARSIPAN guidelines recommend that medical and psychiatric experts work together in managing severely ill people with AN.
The rate of refeeding can be difficult to establish, because the fear of refeeding synrome (RFS) can lead to underfeeding. It is thought that RFS, with falling phosphate and potassium levels, is more likely to occur when BMI is very low, and when medical comorbidities such as infection or cardiac failure, are present. In those circumstances, it is recommended to start refeeding slowly but to build up rapidly as long as RFS does not occur. Recommendations on energy requirements vary, from 5–10 kcal/kg/day in the most medically compromised patients, who appear to have the highest risk of RFS, to 1900 kcal/day.
The term "anorexia nervosa" was coined in 1873 by Sir William Gull, one of Queen Victora's personal physicians. The history of anorexia nervosa begins with descriptions of religious fasting dating from the Hellenistic era and continuing into the medieval period. The medieval practice of self-starvation by women, including some young women, in the name of religious piety and purity also concerns anorexia nervosa; it is sometimes referred to as anorexia mirabilis.
The earliest medical descriptions of anorexic illnesses are generally credited to English physician Richard Morton in 1689. Case descriptions fitting anorexic illnesses continued throughout the 17th, 18th and 19th centuries.
In the late 19th century anorexia nervosa became widely accepted by the medical profession as a recognized condition. In 1873, Sir William Gull, one of Queen Victoria's personal physicians, published a seminal paper which coined the term "anorexia nervosa" and provided a number of detailed case descriptions and treatments. In the same year, French physician Ernest-Charles Lasègue similarly published details of a number of cases in a paper entitled De l'Anorexie hystérique.
Awareness of the condition was largely limited to the medical profession until the latter part of the 20th century, when German-American psychoanalyst Hilde Bruch published The Golden Cage: the Enigma of Anorexia Nervosa in 1978. Despite major advances in neuroscience, Bruch's theories tend to dominate popular thinking. A further important event was the death of the popular singer and drummer Karen Carpenter in 1983, which prompted widespread ongoing media coverage of eating disorders.
(https://en.m.wikipedia.org/wiki/Anorexia_nervosa)
#enoughfortoday #qmo
Labels: Mental Health


0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home